The Central Drugs Standard Control Organization (CDSCO) Registered: CRO/MH/2025/000137
PCOS: Let’s Cure the Incurable!
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders affecting women of reproductive age. The complexity of PCOS presents significant challenges in both diagnosis and treatment. Thus, a comprehensive understanding of PCOS is essential to improve patient care and outcomes. The symptoms associated with PCOS call for a patient-centric approach underscoring the urgent need for innovative and effective therapies by the healthcare sector. This blog explores the real-time obstacles faced while offering treatments and managing PCOS, highlights the critical role of clinical trials in shaping the future of PCOS treatment, and presents the capabilities of RamAayanaM Clinical Solution as your trusted research partner.
1/13/20258 min read
Find the Future of PCOS Care with RamAayanaM Clinical Solution
PCOS is creating a global impact rapidly due to its far-reaching symptoms that may lead to greater complexities if not addressed timely. Considering the current treatment options there are probabilities to innovate in the realm of drug development for PCOS/PCOD management. As clinical trials continue to unravel new dynamics of the causes and optimal treatments for PCOD, Pharma and Nutraceutical industries can be at the forefront of shaping the future of women’s health by conducting clinical research on new molecules and/or combine them with herbs and other botanical ingredients to formulate new and effective evidence-based health solutions.
At RamAayanaM we provide targeted and personalized clinical research approach for a better now and even better tomorrow. New clinical trials can be conducted on existing medications and combinatory drugs to assess their impact on early PCOS/PCOD development. Additionally, nutraceutical investigations by combining latest drugs and botanicals/supplements can let the clinical research industry pave way to developing novel and universal PCOD solutions. RamAayanaM Clinical Solution provides world-class and exceptional clinical research facilities and end-to-end clinical trials for drug development and innovation. Our team of experts are always ready to make sure that the Pharma or Nutraceutical companies get customised solutions for clinical trial investigations of the medicines and supplements for PCOS management and a wide array of therapeutic areas. From hormonal regulation to metabolic health, reproductive support, and psychological well-being, RamAayanaM Clinical Solution with its extensive expertise in preclinical/clinical trials and BA/BE studies, has the potential to play a transformative role in improving the lives of millions of women.
Keep reading to understand the causes of infertility, weight-gain, and challenges associated with PCOS/PCOD diagnosis and management.
Infertility and Associated Diagnostic Challenges in PCOS
The symptoms of PCOS vary significantly based on patient history and lifestyle. Delayed or wrong diagnosis is one of the primary reasons in worsening of PCOS symptoms. As majority of women remain unaware of the condition for an extended period, it often leads to delayed care and treatment. Below are some of the major challenges which are being faced while diagnosing PCOS in women coming from various backgrounds:
1. Reproductive Health Issues based on Age: PCOS/PCOD is garnering attention of the medical fraternity with rising cases of infertility around the world. It causes small cysts around the ovaries, which are immature follicles. This abnormality leads to improper ovulation, thus making the reproductive journey of a woman harder. To top it all, there is no standard diagnostic test or algorithm for the assessment of PCOD patients. However, as per recent consensus of the researchers the Rotterdam criteria has been acknowledged as a standard diagnostic tool for PCOS in women. According to that, PCOS diagnosis can be ascertained in a woman if she shows at least two of the following symptoms: ovulatory dysfunction, clinical or biochemical signs of androgen excess, and/or polycystic ovaries. A notable study suggested that 51.5% of 136 adolescent girls with absolute menstrual irregularity continued to have the irregularity post 2-year follow-up whereas 36% of them were diagnosed with PCOS using the Rotterdam criteria.
Chronic oligo-ovulation or anovulation are key components of the diagnostic criteria for PCOS in adults. But it can be clearly seen that menstrual irregularities and anovulation are becoming highly common in healthy adolescents, complicating the application of these diagnostic criteria in this population. Although menstrual irregularity is common these days, its continuance after 2 years of menarche is deemed clinically suggestive of PCOS/PCOD in adolescent girls.
2. Diagnostic Challenges: The diagnosis can be largely complicated in teenage population and peri-menopausal/menopausal women. One may encounter some PCOS symptoms in adolescents which are typically followed by puberty- such as acne, anovulatory cycles, and oligoamenorrhea or irregular menstrual cycles. Things get further complex while distinguishing ovarian morphology as PCOM is generally observed during puberty as well. Besides, ovarian imaging is not recommended for PCOS diagnosis in adolescents. This sometimes makes it difficult to judge between pathological and routine complications and keeps it challenging for clinicians and the research fraternity to assess PCOS in young girls. A study reported that ovulatory dysfunction in adolescence should be correlated with the absence of menstrual cycle beyond 90 days, or continuous cycles for more than 45 days. While another research suggested that menstrual irregularity in adolescents should be considered upon abnormalities for at least 1 year.
Apart from that, monitoring symptoms, ruling out other endocrine or pathophysiological conditions like hypothyroidism, hyperprolactinemia, non-classic congenital adrenal hyperplasia, Cushing’s syndrome, hypogonadotropic hypogonadism, or even androgen-secreting tumours makes a diagnosis clinically challenging in all age-groups especially women in their 30-40s.
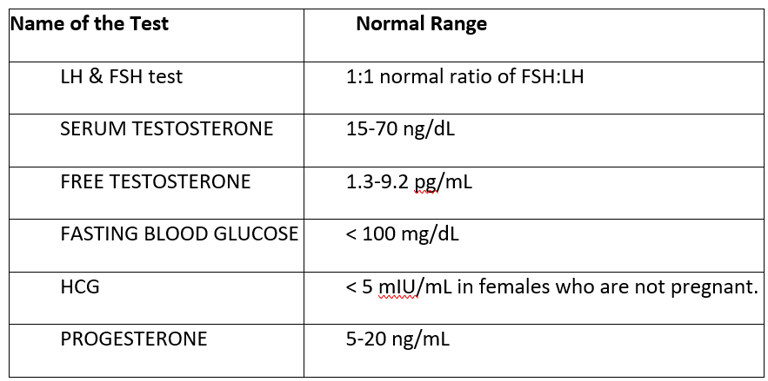
3. FSH and LH disturbances
Women suffering with PCOD show elevated levels of luteinizing hormone (LH) and decrease in follicle-stimulating hormone (FSH). increased LH and decreased or normal FSH levels in PCOS are primarily due to abnormal gonadotropin-releasing hormone (GnRH) and elevated estrogen levels. This causes disruption in the ovulation and menstrual cycle. Clinicians tout the PCOS Panel Test as an ideal diagnostic tool designed to assess key hormones, including LH, FSH, testosterone, and AMH. It helps diagnose PCOS indicators, evaluate ovarian function, and identify hormonal imbalances that may affect fertility. However, LH and FSH values vary depending on the day of the menstrual cycle when they are measured. Therefore, the PCOS Panel Test provides valid results only if the patient arrives on the correct day of assessment. Additionally, obesity influences the levels of these hormones. Hence, the treatment for an obese person coming with hormonal imbalance may conflict with the treatment given for PCOS. Below are the standard values assessed in the test:
Clinical Research for Advancement of PCOS Treatments
Clinical trials are the gateway to drug development and innovation. The complexity of PCOS makes it essential to explore new and improved treatment options for significant outcome and minimal adverse effects. The pharmaceutical and nutraceutical sectors' investment in clinical trials for PCOS treatments is unlocking new possibilities for innovative therapies and effective drugs and supplements. The pharmacological interventions meant to improve fertility include hormone- therapy, ovulation-stimulating drugs, and pharmaceuticals. Below are some notable clinical investigations driving advances in PCOS care:
1. Targeted Hormonal Therapeutic Strategies
Numerous clinical trials are focused on developing more effective methods for regulating hormones. Investigations are underway for advancing hormonal treatments using androgen receptor blockers, selective estrogen receptor modulators, and much more. These clinical studies are focussed on improving ovulation and minimizing skin-associated symptoms like excessive hair growth and acne. Other than that, combination therapies are investigated with anti-androgens and oral contraceptives to overcome the symptoms associated with hormonal imbalance.
2. Improving Fertility Outcome in Women with OCPs, Ovulatory Stimulators & Myo-Ionositol (MI)
Researchers and Pharma industry is a lot more focussed on enhancing the fertility rate in females suffering from PCOS. Oral Contraceptives Pills (OCPs) are already being prescribed to restore the regular menstrual cycles and ovulation, balance out the fluctuating hormones, and mitigate secondary symptoms like acne and hirsutism. However, the symptoms are restored as soon as the dosing stops. Latest drug developments in selective estrogen receptor modulators (SERMs) and GnRH antagonists offer precise treatment for ovulation induction and improving fertility without any significant side effects. Apart from that, advanced ovulation-stimulating agents, in-vitro maturation (IVM) techniques, ovarian drilling procedures, and vaginal progesterone suppositories (PVS) can be tested in various age-groups to make patient’s life easier.
Myo-inositol has also emerged as a promising and evidence-based treatment option for managing multiple aspects of PCOS. Through its positive effects on insulin sensitivity, ovulation, hormonal balance, and mental health, MI offers a multidirectional approach to PCOS care. Past studies on women with PCOS have thrown light on the effectiveness of MI in improving fertility and weight-management. It is also being considered as a viable option for alleviating other PCOS symptoms including stress and depression. Besides, clinical trials continue to provide valuable insights into its role, with most research supporting its effectiveness in improving both metabolic and reproductive symptoms associated with PCOS.
3. Analysis of Effective Biomarkers
Recent research has increasingly focused on identifying potent biomarkers for PCOS diagnosis. Referring to that, Anti-Müllerian hormone (AMH) has garnered significant attention due to its strong correlation with the number of ovarian follicles, making it a significant substitute for ovarian imaging in diagnosis of PCOS/PCOD. Additionally, previous studies identified several regulatory microRNAs that are elevated in women with PCOS. A lot of studies have analysed microRNAs in follicular fluid, while others have examined them in serum. This could render these markers considerably applicable for routine diagnostic use. Some of the identified microRNAs are believed to influence insulin or testosterone levels, both of which typically remain dysregulated in PCOS patients.
4. Metabolic and Insulin-Sensitizing Drugs (ISDs)
PCOS patients may struggle with insulin resistance and weight-gain problems extensively followed by elevated levels of male hormones. Research shows that PCOD women exhibit higher visceral and subcutaneous body fat distribution. Insulin resistance associated with PCOS also increases the chances of type 2 diabetes in women. Here comes the role of Metformin which is a widely acclaimed drug being prescribed as an insulin-sensitizer. Not only that, Metformin also aids in weight management and improves ovulatory function. However, other than Metformin being singly prescribed, new drug combinations are also being studied with and without Metformin for managing insulin resistance in PCOS. Additionally, clinical trials also focus on drugs belonging to GLP-1 receptor agonists, SGLT-2 inhibitors, and thiazolidinediones for the treatment of PCOS-related metabolic dysfunction, and cardiovascular disease. Liraglutide, being used as a second-line treatment for diabetes, is also being touted for weight management and insulin sensitivity and thus, may help in managing PCOD eventually.
Pharmacological Intervention for PCOS Solutions
PCOS is influenced by both genetic and environmental factors, which play a significant role in its development. Till date there is no standard medication for treating PCOD completely; however, early intervention and proactive management is necessary to alleviate the associated risks.
PCOS encompasses multiple aspects of health issues and is a condition which needs to be addressed on time with the right kind of lifestyle changes and healthcare invention. Patient education and innovative solutions with the help of quality clinical research is pivotal in addressing the condition by developing targeted treatments to manage symptoms and enhance the quality of life.
The future of PCOS treatment gets better with RamAayanaM Clinical Solution. Conduct effective and promising clinical trials with us for PCOS therapies and develop advance solutions for more healthier and fulfilling lives.
For more information contact us at +91 9820507220 /+17373134316 or email us at info@rclinicalsolution.com
References
Johnson, P. R., & Davis, L. K. (2024). A trial of metformin versus placebo for the treatment of polycystic ovary syndrome. ClinicalTrials.gov. Identifier NCT04567891.
Smith, J. A., & Lee, M. T. (2024). The effects of diet and exercise on managing symptoms of polycystic ovary syndrome: A randomized controlled trial. Journal of Endocrine Research, 45(2), 123-134.
Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J. S., & Moran, L. J. (2018). International evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction, 33(2), 160-168.
Unfer, V., Facchinetti, F., Orrù, B., Giordani, B., & Nestler, J. (2017). Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocrine connections, 6(8), 647–658.
Legro, R. S., Arslanian, S. A., Ehrmann, D. A., Hoeger, K. M., Murad, M. H., & Pasquali, R. (2013). Diagnosis and treatment of polycystic ovary syndrome: An endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 98(12), 4565-4592.
Agapova, S. E., Cameo, T., Sopher, A. B., & Oberfield, S. E. (2024). Diagnosis and challenges of polycystic ovary syndrome in adolescence. Seminars in reproductive medicine, 32(3), 194–201.
Kambale, T., Sawaimul, K. D., & Prakash, S. (2023). A study of hormonal and anthropometric parameters in polycystic ovarian syndrome. Annals of African medicine, 22(1), 112–116.
Subscribe to our newsletter
Quick Links
Socials
Copyright © 2025. RCS - RamAayanaM Clinical Solution. All Rights Reserved
Registered office
Diva East, Thane, Maharashtra, India
Miami, FL, USA
Branch office
Vikhroli West, Mumbai, Maharashtra, India
Vila Franca de Xira, Portugal
Madrid, Spain
Contact us:
+91-8979335208
+91-9820507220
E-mail:
info@rclinicalsolution.com
bd@rclinicalsolution.com
